HAMPTON CITY SCHOOLS EVERY CHILD, EVERY DAY, WHATEVER IT TAKES!
HEALTH SERVICES

Carrie Battista, BSN, RN, NCSN
Director of Health Services

Jennifer Bowen, RN
Health Services Supervisor

Andrea Rollins, BSBA
Administrative Secretary II
1 Franklin Street Suite 363
Hampton, VA 23669
Phone: 727-2363
FAX: 727-2364

Welcome to Health Services
Hampton City Schools employs registered and licensed practical nurses to provide school-based health services. All are licensed in Virginia and many have bachelors or masters degrees in the field. All of our schools have a full-time nurse. The nurse is responsible for providing care and serving as a medical resource and health consultant for students, parents and staff. The nurse reviews admission requirements, implements specialized health care plans, renders first aid, manages medications, provides in-service training, performs annual inspections, teaches health related topics, and serves as a vital link between parents and health care providers. At our PreK through eighth grade schools, we have, in addition to the RN, licensed practical nurses, LPNs. All middle and high schools have a health clerk that assists in first-aid care and clerical support. All staff are CPR/AED/First-Aid certified.
The primary focus of school nursing is to be an advocate for children’s health and safety within the educational setting. The school nurse’s duties are many and include:
The decision for medical care rests with the parents and parents are always contacted to take their child home or to the doctor as the need arises. Transportation for students is also a parent responsibility. We hope that your child’s school experience will be happy and rewarding. A portion of the school curriculum is devoted to teaching healthy behaviors, which hopefully will become life-long habits and help prevent the need for costly medical care.
“You cannot educate a child who is not healthy, and you cannot keep a child healthy who is not educated.” -Jocelyn Elders
Immunization Requirements for School Entry
Prekindergarten Health Entrance
Kindergarten through Fifth Health Entrance
SCHOOL HEALTH ENTRANCE REQUIREMENTS
All children entering Hampton City Schools for the first time must have a current health examination physical.
Immunization Requirements
Pre-Kindergarten: All state of Virginia four-year-old shots are required for a child to participate in a pre-kindergarten program.
Kindergarten through twelfth grade: All students must adhere to the state of Virginia’s School & Day Care Minimum Immunization Requirements for Entry into School:
Documentary proof shall be provided of adequate age appropriate immunization with the prescribed number of doses of vaccine indicated below for attendance at a public or private elementary, middle or secondary school, child care center, nursery school, family day care home or developmental center. Vaccines must be administered in accordance with the harmonized schedule of the Centers for Disease Control and Prevention, American Academy of Pediatrics, and American Academy of Family Physicians and must be administered within spacing and age requirements.
Diphtheria, Tetanus, & Pertussis (DTaP, DTP, or Tdap) - A minimum of 4 properly space doses. A child must have at least one dose of DTaP or DTP vaccine on or after the fourth birthday. DT (Diphtheria, Tetanus) vaccine is required for children who are medically exempt from the pertussis containing vaccine (DTaP or DTP). Adult Td is required for children 7 years of age and older who do not meet the minimum requirements for tetanus and diphtheria. A booster dose of Tdap vaccine is required for all children entering the 7th grade.
Meningococcal Conjugate (MenACWY) Vaccine - Effective July 1, 2021, a minimum of 2 doses of MenACWY vaccine. The first dose should be administered prior to entering 7th grade. The final dose should be administered prior to entering 12th grade and after the age of 16.
Hepatitis A (HAV) Vaccine – Effective July 1, 2021, a minimum of 2 doses of Hepatitis A vaccine. The first dose should be administered at age 12 months or older.
Haemophilus Influenzae Type b (Hib) Vaccine - This vaccine is required ONLY for children up to 60 months of age. A primary series consists of either 2 or 3 doses (depending on the manufacturer) followed by a booster dose at age 12-15 months. However, the child’s current age and not the number of prior doses received govern the number of doses required. Unvaccinated children between the ages of 15 and 60 months are only required to have one dose of vaccine.
Hepatitis B Vaccine - A complete series of 3 doses of hepatitis B vaccine is required for all children born on and after January I, 1994. However, the FDA has approved a 2-dose schedule ONLY for adolescents 11-15 years of age AND ONLY when the Merck Brand (RECOMBIVAX HB) Adult Formulation Hepatitis B Vaccine issued. The 2 RECOMBIVAX HB Adult doses must be separated by a minimum of 4 months. If the 3-dose hepatitis B vaccine schedule is used, there should be at least 1 month spacing between the 1st and 2nd doses and 4 months spacing between the 1st and 3rd doses.
Measles, Mumps, & Rubella (MMR) Vaccine - Measles, Mumps, & Rubella (MMR) Vaccine - A minimum of 2 measles, 2 mumps, and 1 rubeola. (Most children receive 2 doses of each because the vaccine usually administered is the combination vaccine MMR). First dose must be administered at age 12 months or older. Second dose of vaccine must be administered prior to entering kindergarten but can be administered at any time after the minimum interval between dose 1 and dose 2.
Pneumococcal (PCV) Vaccine: One to four doses, dependent on age at first dose, of properly spaced pneumococcal (PCV) vaccine for children up to 60 months of age. This is not required for kindergarten.
Polio Vaccine - A minimum of 4 doses of polio vaccine. One dose must be administered on or after the fourth birthday.
Varicella (Chickenpox) Vaccine - Varicella (Chickenpox) Vaccine - All susceptible children born on and after January 1, 1997, shall be required to have one dose of chickenpox vaccine administered at age 12 months or older. Effective March 3, 2010, a second dose must be administered prior to entering kindergarten but can be administered at any time after the minimum interval between dose 1 and dose 2.
Human Papillomavirus (HPV) Vaccine - Effective July 1, 2021, a complete series of 2 doses of HPV vaccine is required for students entering the 7th grade. The first dose shall be administered before the child enters the 7th grade. After reviewing educational materials approved by the Board of Health, the parent or guardian, at the parents or guardians sole discretion, may elect for the child not to receive the HPV vaccine.
![]() Medication at School
Medication at School
General Information
If your child is on medication, it is recommended that arrangements be made with the prescribing doctor so that the medicine may be taken before or after school hours. If this is not possible, please see the information below to ensure you are in compliance with HCS medication policies. If you have any questions please contact your school’s nurse. It is the responsibility of the parent to provide refills as necessary throughout the school year and to pick up all unused medication at the end of the school year. Medication not picked up will be discarded.
Please note the following:
Medication Request Form SBO 23 pdf
Carrying Medication:
Students may not possess medication at any time during school hours or activities. Exceptions may be made for those students who require certain inhaled asthma medications, self-injected epinephrine, or other emergency medication. Student possession of such emergency medications shall require an additional form signed by a physician, parent, student, and the school nurse. Students who abuse this privilege may lose the ability to carry and self-administer medications.
Authorization to Carry and Self-Administer Medications (SBO 28)
Authorization to Carry and Self Administer Epinephrine (auto-injector)
Important Forms/Information for Students with Life-Threatening Allergies:
Parent and Student Responsibilities for Life-Threatening Alleries
Checklists for Parents of Students With Life Threatening Allergies
Other Medication Issues & Forms:
Children with Asthma and/or Life Threatening Allergies require special written health care plans completed and signed by their health care provider and co-signed by their parent/legal guardian:
Children with asthma may need an Asthma Action Plan (AAP) especially if medication is kept in the school and/or hand carried. The Asthma Action Plan helps to manage your child’s asthma. At school, the Asthma Action Plan tells school staff which medications to use to prevent and/or respond to asthma emergencies.
Children with life threatening allergies may need the Life-Threatening Allergy Management Plan (LAMP) especially if they have medication in the school and/or hand carry medication. The Life-Threatening Allergy Management Plan helps to manage your child’s life threatening allergic reactions. At school, the Life-Threatening Allergy Management Plan tells school staff what to do to prevent (such as avoiding the child’s allergens) and/or respond to life-threatening allergy emergencies.
Children with Seizure/Epilepsy may need a Seizure Action Plan especially if they have medication in the school.
Medications for After School Activities/Events:
In regard to emergency medications a student may need available for after school activities/events, it is extremely important parents/guardians notify the individual in charge of the activity/event about this need. Examples of emergency medications include Epi-Pens ®, insulin, glucagon and asthma inhalers. After regular school hours, the clinic is closed and a nurse is not available. Prescribed medication in the clinic cannot be used for before or after school activities. It is the parent/guardian’s responsibility to provide the medication and develop a plan with the individual in charge of the before or after school activity/event so a safe environment may be maintained. The school nurse can provide a copy of the doctor’s order and assist in training, if needed. Please note a student may carry emergency medications when the proper procedure is followed as stated above. It is the parent/guardian's responsibility to develop a plan with the nurse and the individual in charge of the after-school activity/event so a safe environment may be maintained.
Eating Disorders
Should my child stay home from school?
No, if he/she has…
Vague complaints of aches, pains or fatigue
Sniffles or a mild cough without a fever
A single episode of diarrhea or vomiting without other symptoms
Yes, if he/she…
Has a temperature of 100.4° or higher. Keep them home until fever-free for 24 hours without medicine. Never give aspirin to a child under 19 years old. If has had two or more episodes of diarrhea or vomiting must remain out 24 hours once symptoms have stopped without medication.
When your own judgment tells you that your child is not well. If you suspect your child may be ill, delay sending them to school until you have had enough time to observe their behavior and feel certain that they are well enough to be in school.
Your child has been diagnosed with a contagious illness and has not yet received medication for a minimum of 24 hours, or until your doctor tells you your child is no longer contagious.
A red eye with white or yellow discharge or matted eyelids after sleep
An earache
Constant, thick nasal discharge
A sore throat, so bad that your child will not eat or drink
A persistent productive cough or wheezing
More than one episode of diarrhea or vomiting
An undiagnosed rash or spot
Chicken Pox. Your child may return when all of the blisters are scabbed over and dry.
Extreme fatigue
A lot of pain for some reason (for example, a new injury)
Head Lice. Your child may not return until treated and no live lice. Parent/Guardian must bring student to the school nurse to be checked before returning to class.
Hydration Tips
During the summer months, children as well as adults enjoy many outdoor activities. These activities put people at a greater risk for dehydration and heat stress. Dehydration is the loss of both body water and electrolytes which are vital to the function of the human body. Not having enough water and electrolytes interferes with normal body processes and can lead to a serious and potentially fatal condition. The following are warning signs of dehydration and heat stress: fatigue, lethargy, rapid breathing, tenting (if the skin does not bounce back readily when lightly pinched and lifted), dark colored urine, low or no urine output, headache, and the inability to produce tears.
The best defense in the prevention of dehydration is proper hydration.
Here are some tips to help you and your child to stay well-hydrated:
1. Drink a minimum of eight glasses of water each day. A person who is more active will require even more water to properly rehydrate.
2. Drink plenty of fluids throughout the day. Don’t wait until you are thirsty to drink water. By the time a person becomes thirsty, they have probably lost two or more cups of their total body water composition.
3. Don’t substitute other beverages that contain caffeine and alcohol for water. Although all beverages help to hydrate the body, beverages containing caffeine and alcohol act as diuretics and cause loss of water by increasing urination.
4. Begin and end your day with water. Even while we sleep, we lose water.
5. Drink water throughout exercising. During a workout, take frequent water breaks. Many people underestimate the amount of fluids lost with perspiration.
6. Drink cool water instead of carbonated beverages or sports drinks for keeping hydrated when it is warm outside. Cool water is absorbed more quickly than warm fluids. Save the sports drinks for the long training sessions or for after exercise is completed.
7. Don’t forget that illnesses, such as the common cold, flu, etc. cause water loss that frequently leads to dehydration. Keep a bottle of water by your bedside and sip on it throughout the day if you are home sick.
 Diabetes Information
Diabetes Information
Helpful Information
• CHKD diabetes
• Parent and Student Responsibilies for handling diabetes in the school setting
• Parent Checklist
• Virginia Diabetes Medical Management Plan
• Parent Contact Form
• VA Diabetic Medical Management Plan
• Intensive Therapy
 • Pump Therapy Supplement
• Pump Therapy Supplement
• Permission Self Carry
• Virginia DM Management Protocols
• Diabetes Tracking Record
Resources
• Pharmaceutical Assistance
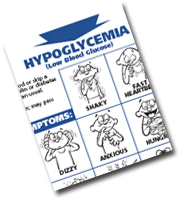
• Signs and Symptoms of Hypo/Hyper-glycemia (PDF)
• Helping the Student with Diabetes Succeed (PDF)
• Diabetic Tracking Record (PDF) or (XLS)
• Diabetes Support Groups: Children's Support | Yearly Diabetes Camps
• Diabetes Care Tasks at School: What Key Personnel Need To Know
Returning to School after an Injury or Surgery
Hampton City Schools (HCS) is committed to ensuring the health and safety of our students. It is important for the nurses at HCS to be aware of anytime a student has been injured, whether at school or at home, which might require any change in the academic day. Please review the following medical issues that may require additional information before your student returns to school.
Concussion/Head Injury:
If a student has sustained a concussion or brain injury diagnosis by a coach/athletic trainer or medical provider, the following things MUST be completed prior to returning to school. It is also important to know if the student has sustained multiple concussions.
Injury requiring any orthopedic device (crutches, boot, cast, etc.):
Surgery, minor and major:
Any surgery can impact a student’s academic day. The following information should be reviewed before the student returns to school.
Special Forms
• Special Dietary Needs
• Enteral Feeding Oders
• Oxygen plan
• Chronic Illness Verification form
RESOURCES FOR CHILDREN/FAMILIES WITH NO HEALTHCARE INSURANCE
Encourage them to apply online or call to see if they qualify for FAMIS/Medicaid through Virginia’s CardinalCare Program. coverva.dmas.virginia.gov or 1-855-242-8282 A family of four can earn up to $65,908 and still qualify for coverage (amount increases with each additional family member).
Health care providers for all ages
Southeastern Virginia Health System (formerly PICH)
4 locations in Newport News VA
Call 757-380-8709 for appointment; dental care also available
Open M-F 8:00am-5:00pm
BonSecours Care A Van
Location changes daily throughout Peninsula/Tidewater areas, calendar is available online
https://www.bonsecours.com/locations/community-services/hampton-roads/care-a-van
Call or email Ms. Takeirah Martin for more information 757-889-5121 Takeirah_Martin@bshsi.org
Charlie & Golden Bethune Community Health Clinic (part of Riverside Medical Group)
727 25th St. Newport News, VA 757-316-5210 https://www.riversideonline.com/locations/primary-care/charlie-w-and-golden-bethune-hill-community-health-clinic
They provide an initial 50% discount for clients without insurance and then clients can apply for financial assistance
Health Care providers for Adults only
Lackey Clinic
1620 Old Williamsburg Rd, Yorktown VA 757-886-0608
Virtual visits available; apply online to become a patient; dental care also available
EVMS HOPES Clinic
Norfolk Dept. of Public Health Building, 830 Southampton Ave, Norfolk 757-446-0366
https://www.evms.edu/education/resources/community-engaged_learning/hopes/
Mental health care for all ages
Hampton-Newport News Community Services Board (CSB)
300 Medical Drive, Hampton VA 757-788-0300
Provides a wide variety of care, including walk in services, medication management, crisis intervention, support for people experiencing homeless, support for people with developmental disabilities
Vision care
https://childrenseyefoundation.org/what-we-do/all-children-see/ Parents complete an online application
https://new-eyes.org/application Eyeglasses only. School Nurse can complete for parent; parent can also complete; must have a prescription dated within last 24 months that includes PD (pupillary distance)
https://respectacle.org/index Eyeglasses only. Must have current prescription; finds glasses (that have been donated) in stock that match prescription as close as possible and recipient chooses from the options provided
School Health Advisory Board
Mission Statement:
The School Health Advisory Board shall assist with the development of health policy in the school division and the evaluation of the status of school health, health education, the school environment, and health services.
Purpose:
The School Health Advisory Board for Hampton City Schools shall advise, support, and assist with the development of effective board practices and procedures, review relevant school health policies, foster family and community support and involvement in developing and implementing school health programs. This will include health instruction, healthy school environment, school health services, school counseling, physical education, family life education, school services, and health promotion for staff members.
SHAB Contact person:
Edwina Forrest
Food and Nutrition Services
Hampton City Schools
Hampton, VA 23666
757-727-2350
eforrest@hampton.k12.va.us
The Impact of Opioids
In Virginia, drug overdoses are the leading cause of unnatural death and have been since 2013. More Virginians die every year from overdoses than from automobile crashes. Opioids - specifically fentanyl - has been the driving force behind the large increases. In 2021, fentanyl contributed to 76.4% of all Virginia overdose deaths. It was estimated that 98% of these fatal fentanyl overdoses in Virginia were caused by the illicit, rather than prescription, version of the drug. Awareness and education are two of the best defenses against opioid misuse and overdose.
The U.S. Department of Health and Human Services, National Institutes of Health (NIH), provides important information on Opioids and the devastating impact that the drug epidemic is having in communities and schools. Resources include data on the current impact of opioids, research on drug use and addiction, overdose prevention, and opioid overdose reversal medications.
The Virginia Department of Health provides primary and overdose prevention strategies in English and Spanish, Virginia-specific drug overdose and health-related data, health impact data, and provider training and education.
Drug Education and Prevention Programs
Local school divisions and parents seeking information for students to develop good decision making skills and prevent violations of Virginia law may consider the following:
Federal Programs and Resources
One Pill Can Kill: The United States Drug Enforcement Administration (DEA) created this campaign to encourage the use of social media to help raise public awareness of a significant nationwide surge in counterfeit pills that are mass-produced in labs, deceptively marketed as legitimate, and are killing Americans at an unprecedented rate. Virginia Attorney General Jason Miyares and First Lady Suzanne S. Youngkin launched Virginia’s "One Pill Can Kill” public awareness initiative in November 2022 to help generate open, honest conversations amongst families about the extreme threat that counterfeit drugs and opioids pose.
Substance Abuse and Mental Health Services Administration: SAMHSA is the agency within the U.S. Department of Health and Human Services leading public health efforts to advance the behavioral health of the nation. SAMHSA provides multiple resources on the warning signs of opioid overdose and how naloxone and medications for OUD treatment can help treat and prevent it.
National Institute on Drug Abuse: NIDA, under The National Institute of Health (NIH), is the lead federal agency supporting scientific research on drug use and addiction and provides data and resources on Opioid use.
Virginia Programs and Resources
Virginia Rules: Virginia Rules is an educational program especially designed to help instructors, parents, and students understand the laws that apply to Virginia teens in their everyday lives. Information includes violations and penalties regarding possession, sale, distribution, or manufacturing of opioids in the school setting.
Curb the Crisis: Curb the Crisis features information about where to seek treatment for opioid misuse for yourself or a loved one. Alongside the latest research and data on the opioid crisis, it also contains information on referral and treatment services in Virginia.
Substance Use Disorders and Opioid Addiction in School Communities: The VDOE Virginia Career and Learning Center for School Mental Health Professionals offers professional development and career opportunities for school counselors, school social workers, school psychologists, and other licensed school mental health professionals in Virginia Public Schools.
This nine module training series provides school divisions and relevant stakeholders with important information on opioid overdose prevention, effective approaches, and access to care.
State Opioid Treatment Authority (SOTA): Each state has a designee that plays a key role in providing oversight and support to the opioid treatment programs that use methadone and other Food and Drug Administration-approved medications and provide counseling and other services to individuals with opioid use disorder. For Virginia, the SOTA is Diane Oehl - diane.oehl@dbhds.virginia.gov.
Additionally, Hampton City Schools School Social Work Department has created a Hampton Roads Resource Guide. This guide may be helpful for families seeking mental health support for drug use and addiction.
Parent Notification
Please note that often medical events require medical and/or law enforcement investigations to determine what occurred. While we recognize that it is important to notify families as quickly as possible, the Virginia Department of Education recommends that the school division allow the medical and law enforcement professionals to medically/scientifically verify that the student emergency is a school-connected student overdose.
As such, Hampton City Schools will utilize a ParentSquare post (email) to notify all HCS families of the respective school once a school-connected student overdose is confirmed by a medical and/or law enforcement investigation.